Conversations with Rich Bennett
Join Rich Bennett and his dynamic cohosts as they engage with individuals from diverse backgrounds—authors, entrepreneurs, activists, and everyday heroes—uncovering their unique stories and insights. Each episode offers a deep dive into personal journeys, community initiatives, and transformative experiences, providing listeners with inspiration and practical takeaways.
Tune in to discover stories that uplift, inform, and connect us all. Subscribe now to be part of these compelling conversations.
Interested in being a guest on Conversations with Rich Bennett? Reach out to Rich Bennett through PodMatch: https://www.podmatch.com/hostdetailpreview/richbennett.
Conversations with Rich Bennett
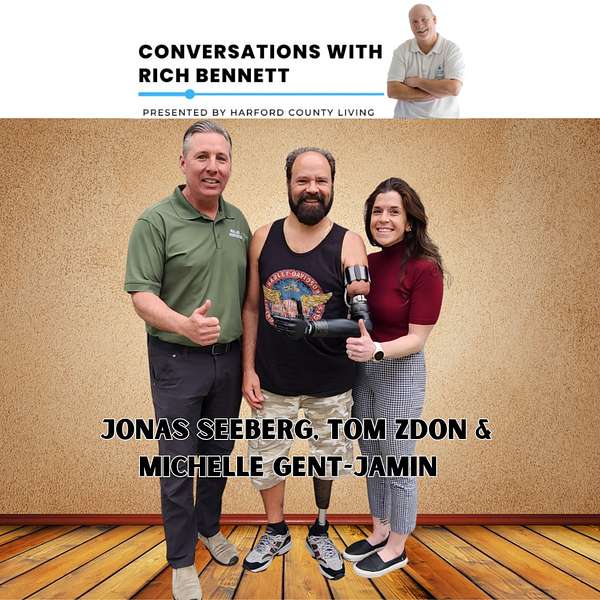
Tom Zdon's Life with Cutting-Edge Prosthetics
In this enlightening episode of "Conversations with Rich Bennett," sponsored by Eco-Cool HVAC, host Rich Bennett engages with three remarkable individuals in the field of prosthetic technology. Tom Zdon shares his empowering story of adopting an advanced prosthetic arm after a life-altering accident, highlighting the enhanced functionality provided by COAPT's control systems that interpret neural signals. Jonas Seeberg, owner of Real Life Prosthetics, discusses the customization and personalization of prosthetics that cater to individual needs, enhancing users' quality of life. Michelle Gent-Jamin, from Align Rehabilitation, adds depth to the conversation by explaining the rehabilitation process and the critical role of tailored therapy in integrating prosthetics into daily life. This episode sheds light on the technological advancements, personal triumphs, and collaborative efforts shaping the future of prosthetic technology.
Here are links for you to bookmark, save, follow, memorize, write down, and share with others:
Real Life Prosthetics™ | Restoring Real Life Ability Since 2001
Align Rehabilitation | Amputee Physical Therapy Specialists | MD & DE (alignrehab-pt.com)
This episode is sponsored by Eco-Cool HVAC
Eco-Cool HVACYOUR FRIEND IN THE SUMMERS & WINTERS! Heating & Air Conditioning Service and Repair, Furnace & Boil
Disclaimer: This post contains affiliate links. If you make a purchase, I may receive a commission at no extra cost to you.
Rate & Review on Apple Podcasts
Follow the Conversations with Rich Bennett podcast on Social Media:
Facebook – Conversations with Rich Bennett
Facebook Group (Join the conversation) – Conversations with Rich Bennett podcast group | Facebook
Twitter – Conversations with Rich Bennett
Instagram – @conversationswithrichbennett
TikTok – CWRB (@conversationsrichbennett) | TikTok
Sponsors, Affiliates, and ways we pay the bills:
Hosted on Buzzsprout
SquadCast
Rich Bennett 0:00
So how are you guys doing, first of all?
Good.
Jonas Seeberg 0:04
We're doing really good in our journey. So I know last podcast we were talking about the relationship that real life prosthetics has with Align rehabilitation and our goal of establishing independent space for our companies to work in. So since we spoke with you last, we are in real life prosthetics is looking to expand its lab into the suite next door. Oh, wow. We have expanded real life prosthetic or align rehabilitation is having their grand opening the beginning of May. So May 3rd. So we're hoping to have a lot of people there. And it will be nice to take those in the community on a journey of the design of prosthetics, the fabrication of prosthetics. Right. How prosthetics interface patients, how prosthetics transforms our patients lives, and then their journey through the rehab process. So we're hoping to have patients there and hoping people can come through and just have an eyewitness account of patients that we've worked with and we've collaborated on to restore independent ability.
Rich Bennett 1:11
And you guys brought a special guest this time, right?
Michelle Gent-Jamin 1:15
We did.
Rich Bennett 1:15
We did. She speaks.
Michelle Gent-Jamin 1:17
I didn't see I didn't want Jonas. I mean, I don't want to interrupt him, But yes, I made my third my half birthday, which is also real life prosthetics. 23rd, 23rd anniversary of Operation will be our open house. And so, yeah, we took the suite align rehab, took the suite directly next door to real life, and I designed it to be really as the most supportive environment for my amputee patients specifically. So we installed a overhead track harness where I'm able to kind of harness someone up who might be a little less confident standing up. And that way we can start training outside of parallel bars, start training, going upstairs and ramps, but with the security of being harnessed. So that was super exciting. So, yeah, May 3rd, everyone is invited to come see that space. And then you can see real life lab where part we call it like the clean lab, and then you go into the dirty lab where there's more grinding and sanding and dust particles and all the way through its final. And I want to say, what am I saying? Final project.
Jonas Seeberg 2:41
Final
fabrication. Yeah, Like the device. Yeah. Yeah. So we have our dirty, dirty space. It is for pulling of plastic lamination, grinding carbon fiber filaments, vacuum evacuation systems, and then into the clean space could be the assembly touch ups, small adjustments. And the clean space is what sits behind a line. Rehabs gym. Okay, so we wouldn't want the dirty space and all that dirt going in to. Right. Jim, did.
Rich Bennett 3:11
You make sense?
Jonas Seeberg 3:12
Have people breathe in?
Rich Bennett 3:14
You said half birthday.
Michelle Gent-Jamin 3:16
Oh, yes.
Rich Bennett 3:17
What is a half birthday?
Michelle Gent-Jamin 3:19
It is exactly six months from my real birthday, which is November 3rd.
Rich Bennett 3:27
Well, never mind.
Michelle Gent-Jamin 3:28
It's okay.
Rich Bennett 3:29
That's all right.
Michelle Gent-Jamin 3:29
But, yeah, we did. We brought a special guest. Tom's it on. Tom has been a long time patient of real life prosthetic. And then most recently, I've been able to to start working with him after his ICU integration surgery. I will have Tom introduce yourself. How cool you are. All the things you do and all the cars you have.
Rich Bennett 3:53
We've met one car collector. Yes.
Tom Zdon 3:57
Oh, I was.
Rich Bennett 3:58
I was
just going to make me cry. Is it?
Tom Zdon 4:03
No. No.
Rich Bennett 4:04
Okay. All right. How you doing, Tom?
Tom Zdon 4:06
I'm doing good. I'm doing good. My name's Tom Zadan. I grew up in Harford County. I've always lived here. I went to Aberdeen High School, so Jonas is definitely a plus for me. Being close.
I was in a bad accident five years ago. I lost my left leg, my left arm. Oof! In the accident. Was it shock? Trauma? You know, life. Life goes on.
Rich Bennett 4:36
Right?
Tom Zdon 4:37
You can't. Nobody's going to baby you or anything. Everybody's different in the way they think. So it's upon yourself to do what you're going to do in life. So for me, I've been a very active carpenter in my life. I worked at a cabinet factory for over 20, over 20 years.
Rich Bennett 4:58
Wow.
Tom Zdon 4:58
So I enjoyed hot rods, cars, boats, motorcycles. My accident was on a motorcycle, and fortunately, a guy hit me head on.
Rich Bennett 5:08
Oh, man.
Tom Zdon 5:10
Took my wife. Any accident over 24 years.
Rich Bennett 5:13
Oh, God.
Tom Zdon 5:14
So you got to be pretty much enjoy every day. You never know what's going to happen from day to day.
Rich Bennett 5:23
And this was five years ago.
Tom Zdon 5:24
This was almost five years ago. July 5th, coming up. So I live out in the country. I got a big yard swimming pool. Like you said, I've always been active. I had a bunch of hotrod cars. I always grew up with hot rods and stuff
and then motorcycles. Always been a motorcycle rider, been through many journeys from Florida to California to to Maine. I rode everywhere. I think I trail at one time and didn't like it.
Rich Bennett 5:54
So no sort of better ride, man. It just feel so good.
Tom Zdon 5:57
So. So. But being a double amputee, there is a possibility maybe one day. But the way motorcycles are going and the traffic, it's not for me. I don't want to try to kill somebody.
So it's it's a new chapter in life.
Rich Bennett 6:17
Yeah.
Tom Zdon 6:18
I got to think of things to do and do something different. So I had a lot of hotrod cars. Some cars had clutches missing my left leg, so I wound up selling them.
Just never like to drive. So I was always buying something different
cause the wife didn't like it. But I mean, it is what it is. Yeah, but, I mean, I have. I have a nice piece of property. I live on a golf course. I have little over an acre. I cut my own grass
and I have a swimming pool. So a lot of people always question me. How how do you do that with without your arm and leg? Well, I mean, if there's a will and you want to do it, you got to just go do it.
Rich Bennett 7:08
Sounds familiar.
Tom Zdon 7:09
So for me, I feel like I'm 56 years old. I feel like I'm in good shape. Yeah, I'm healthy. I'm just missing my arm and leg. So. So I'm out there. So I'm definitely enjoying the summertime coming now because I'm able to get outside the grass, open the pool up. I can get in the water because that's probably one of the best therapies you can have being an amputee to get in the water because it's light feeling. You don't have to worry about falling. You can get in exercise. So so I have an above ground pool. I have a wheelchair, but I haven't actually used my wheelchair in probably four and a half years.
Rich Bennett 7:50
Really, ever.
Tom Zdon 7:50
Since I got out of the.
Rich Bennett 7:51
Hospital. Okay. I don't know if that's a good thing or not, because Michelle's life.
Michelle Gent-Jamin 7:55
Is an amazing.
Rich Bennett 7:56
Thing. Okay, That's what I thought.
Tom Zdon 7:58
I mean, like I said, it depends on each person.
Rich Bennett 8:00
Yeah.
Tom Zdon 8:01
How they feel. I do not try to hop because I don't want to hurt my good leg.
Rich Bennett 8:06
Right.
Tom Zdon 8:07
So I do have a small kind of a tractor shop stool that I sit on because my house has a small hallway. So I do sit on that when I don't have a leg on. Mm hmm. But usually by 9:00 in the morning, I'll put my leg on and it's on till 11:00 at night.
So I take it to the extreme. But who doesn't want to not have a leg on?
Rich Bennett 8:31
Right?
Tom Zdon 8:32
You know, I want this leg to be my own leg again. And as time goes on, it does start feeling better. But it's it's a rough period. You know, some people can't cope with it then some people can.
Rich Bennett 8:46
Yeah.
Tom Zdon 8:47
For me, I've the way I grew up, my dad was hard on us. So if we weren't kicked in the butt to get out and do something, you know, I can still hear him from heaven, you know, yelling at me.
Rich Bennett 9:02
That's good.
Tom Zdon 9:02
Let's do it. Get out and do it.
Rich Bennett 9:04
Yeah, My parents were the same way.
Tom Zdon 9:06
And so it's it's a different generation now. But. But yeah, with amputees, I mean, I try to help. I've been to a couple different amputee meetings. I used to go to Upper Chesapeake and Bel Air. Mm hmm. I still go to their monthly meetings and I try to help some of the amputees that are there. But most of them I can't relate with because they are diabetes people, maybe in their 6070s. So they have different issues.
Rich Bennett 9:35
Right?
Tom Zdon 9:37
But I try to help them out. And, you know, they're the only one that is going to be able to help themselves. You can have somebody every day telling you, do this, do that, But if you don't have it in your mind to do it or you don't want to do it, you're never going to know. For me, I have to be out every day. My leg is going to be on me. Maybe not so much my arm, but in order for me to drive, to get out, walk, you know, do anything. If I don't have a leg, then I'm pretty much grounded.
Rich Bennett 10:07
So now, when when you go swimming. Yes. Can you wear the arm in the leg in the pole?
Tom Zdon 10:13
I cannot.
Rich Bennett 10:14
Okay.
Tom Zdon 10:14
Yet the arms are. No, but there are some legs that you can. But it's the way it gets hooked on to your body.
Rich Bennett 10:22
Right. Okay.
Tom Zdon 10:23
So there is different strap systems I could wear and be able to do that. Maybe one day we can basically just kind of like a peg leg. Yeah, Something that just has something there for you.
Rich Bennett 10:35
That's all I said. Yet because I do Analogy thread two years. It's just amazing here.
Tom Zdon 10:39
Because I am a water person. I've always I've always had a boat. I've always been swimming in the bay, you know, the Susquehanna River. I'm a water skier and as of last year I was still out on my boat without an arm and leg water skiing. Wow. You know, nobody wants to pull me because they're scared to death. They're going to hurt me. But maybe I need to get a remote control. But just do it myself.
Rich Bennett 11:05
I would if I had a boat, I'd pull you, Tom, in a heartbeat. So if Michelle. So that's okay.
Tom Zdon 11:11
But you can't be scared of the water, right? Do you have any fear of it? Then you shouldn't be in the water.
Rich Bennett 11:16
Well, yeah, and that's a funny thing. You'll have some people say, Well, you have to overcome your fears. Well, there are limits to this, you know, on how you do that. Yeah. So after the actually you say you were how long were you in shock trauma for?
Tom Zdon 11:31
I was in shock trauma for almost 30 days. Okay. I was out for almost a week when I woke up. Wow. You know, they given me so much blood that it was beyond the point of living. Wow. I mean, Doctor, Dr. Scalia, which is the head of Sharp trauma.
Rich Bennett 11:51
Yeah, I've heard his name.
Tom Zdon 11:52
He is the one that actually worked on me. And everybody was amazed that after a week I woke up. And when I woke up, I was ready to go. You know, I was up trying to stand up. I was just ready to do it, you know? I mean, there's nothing can bring back your arm or leg.
Rich Bennett 12:09
Right.
Tom Zdon 12:10
But so so I went through that period of time. I think I've been through 16 surgeries now with infection. You know, they had to keep cutting and cutting and then, you know, and now with my arm, I think I've been through three or four surgeries to better myself to have this eye that I have now, osteo integration. So so it definitely makes life a lot better for amputees if you're able to have it. So I currently have it in my arm and I'm currently looking into possibly getting it in my in my femur bone in my left leg. You know, I yes, you.
Jonas Seeberg 12:48
See, that's above the.
Tom Zdon 12:49
Knee. So that would that would change a lot up. I currently have a.
Jonas Seeberg 12:57
A locking line, a locking.
Tom Zdon 12:58
Liner with a strap. So it's hard for me to put it on with one hand. It's kind of like a wet suit material that has to roll on.
Rich Bennett 13:07
Oh, wow.
Tom Zdon 13:08
So I kind of struggle with that. But I mean, it's it's capable. I mean, there's if there's a will, there's a way, right? You can do a lot of things with one hand, and I do. And one other thing to point out is I was left handed, so it took my dominant hand from me. Oh, so now. But being in the carpenter world, everything tools are everything's pretty much designed for right hand.
Rich Bennett 13:31
Right.
Tom Zdon 13:31
So I guess I'm a chosen. I'm a chosen one. Know.
Rich Bennett 13:36
Well, because when you guys came in and I saw those of you listening, his left arm, I want to say what is bionic, right? It is. I mean, little fingers. Everything's. You can move it in all. Which like the old prosthetics you can do that with. Now with your therapy. Are you are you doing anything where you're trying to learn how to use your left hand again, as far especially with the wood?
Tom Zdon 14:04
Oh, yes. Yes. I'm learning right now to pick up things and kind of be a little more sensitive when I grab things. Right now, it's basically a I don't know how you would call it, like open and close. I don't have individual fingers. Okay. I can move, but you can do different settings within operation of it. So there are sensors that I don't feel how strong arm grip in it, but it's kind of like building a seventh sense. Mm hmm. You learn. You learn. It's like it's. It's kind of like saying, like, when you're eating dinner and you get something with your fork, you know where your mouth is, right? So it's. It's kind of like connecting to you after a period of time.
Rich Bennett 14:53
So with this general, as you probably answer, answer is with your arm, because you got that being. I take it these are sensors up there that connect to the nerves. Yes.
Jonas Seeberg 15:05
Yes. So in a traditional myoelectric prosthesis, like a socket build. Mm hmm. If we back up, you know, five years, four years, the way that the amputee would control prosthetic elbow, wrist and hands would be through two sensors that would be embedded into the prosthetic socket. So an amputee puts the socket on. Right? You would have two sensors that are touching the skin over muscles that provide the strongest signal. And for an above elbow amputee like Tom, he has a very complex system. So through the microprocessor electrodes that are embedded into the socket, his muscles will send signals to the different motor systems in the elbow and the wrist and the hand.
Rich Bennett 15:59
Wow.
Jonas Seeberg 15:59
But the old system was very complex because you only had the two sites for sensory. So in order for Tom, if he had this old system to jump between sensors, he would have to contract his muscles in a certain way. Basically, like making making a strong muscle. Mm hmm. So if he wanted to bend his elbow, the front part of the arms called, you know, our biceps, he would he would flex his bicep, and then the the electrodes would send the signals to the microprocessor system, then would drive the elbow to bend the elbow and bring the hand toward the mouse. And then if he wanted to straighten the elbow, he would have to tighten his tricep muscle. And then that tricep muscle would send the signal to the electrode, to the microprocessor sensor system to the elbow, and then he would straighten. So he's in this realm of only controlling the elbow. Okay. Okay. Now he gets the elbow to the correct position. Now he wants to rotate his wrist so he would have to do what we call a co contraction. So he would have to flex both muscles in fast succession like boom boom. And then that would jump the microprocessor signal from the elbow down to the wrist. And then he would use biceps, triceps to rotate the wrist downward upward. Then he'd have to do like a triple contraction boom to jump the motor down to the hands, to open, to close. So for upper extremity amputees, the old myoelectric systems are very complex, right? And unfortunately, most end up in the closet because it takes a lot of drive and determination. I believe somebody like Tom, he would master it.
Rich Bennett 17:42
Right.
Jonas Seeberg 17:42
But but but for most, you know, you do end up seeing the prosthesis in the closet. And then they they revert into a single handedness and then they run into overuse syndrome. And there's all kinds of things that happen with their sound side because they're overusing their arm. So fast forwarding to today, and with Tom's design, he has a very unique sensor system. It's made by by Coapt. So the technology in the elbow, the wrist and the hand are the same. But the way the signals are picked up from the residual limb or the way that those signals are transferred into the different systems occur automatically. So the easiest way to explain these two different systems, old and new, is think of a symphony orchestra. Mm hmm. All right. So you have you have your woodwinds. You know, you have your your cellos and you know, you have your strings and your violas and your violins and your woodwinds and your oboes and your clarinets. And you have it just just think that you're sitting in a symphony hall and you're listening to a master piece of music and try to pick out the oboe, try to single out that one instrument.
Rich Bennett 18:55
Right.
Jonas Seeberg 18:55
It's very difficult to do because there's so many instruments making noise. Well, that's the old microprocessor system. So you had software and it was trying to pick up a specific instrument within that orchestra to control the different parts of the arm. So it's hum. And with Coapt, now you're at that symphony. This system is designed where there's instead of two electrodes set up on his arm there, there's 16 electrodes. Wow. And a ground. So there's there's six, there's 17
little like mushroom heads integrated into the specialized band, which goes on to Tom's residual limb that push into his arm. Wow. So now what we've done is we've created an antenna network all the way around his arm. So now we're listening to the entire symphony play and we're listening to the songs that are being played. So with with Michel and I working together, we're basically and Tom as well, we're learning the different notes are the different songs that are being created. And he's he's making his own songs for those different functions. So it would almost it's close to where his, his arm, you would hear is like a thought process based arm. Mm hmm. And Michelle and I are working together with Tom, their specialized software that we use. So what we'll do is to sit down with Tom, and. And we'll get into the different points of operation in his arm. So we have six different motions. So we have the elbow bending, straightening wrist rotating in one direction or the other. Hand's opening and closing.
So what we'll do is we'll isolate each of those individual motor functions. So say, for example, we'll start off with the elbow bending to bring his hand to his mouth and the programming will call. We'll do what's called mapping. Mm hmm. So the the electrodes on his arm, the 16 sensors are listening for the muscle function throughout his entire arm, biceps, triceps, whatever muscles are being used. Tom is going to think in his mind's eye that he's bringing his prosthetic hand up to his face, bending the elbow. And as he's thinking that on the computer screen, we can see the mapping of that of that song.
Rich Bennett 21:35
Right.
Jonas Seeberg 21:36
And then once we get a strong mapping of the song, then we will isolate that thought to bending his elbow and bringing his hand toward his mouth.
Rich Bennett 21:45
Wow.
Jonas Seeberg 21:45
And then we can refine that. So we we can continue to add to that mapping into that muscle pattern, which would drive the motor for that specific function. And then we take him through for straightening the elbow, rotating the wrist downward, which we call wrist pronation, rotating the wrist upward, which would be supine, Asian hands, open and close, and then back to straightening the elbow. So that's how the system works. It's very advanced. And back to the contractions, he's not having to do a double contraction. Triple contraction. He's simply thinking of the motion that he wants out of the arm. And the Coapt technology will then send those signals to the microprocessor, which will automatically jump between motors, between elbow, wrist and hands. So now we have amputees who can successfully use prosthetic arms. And we're seeing, like the likelihood that they do not end up in the closet. Now, I want to back up with Tom's arm, his his old arm and the socket design. So before I ask you, integration, most amputees out there, they have a socket that they have to slide their residual limb down into the socket. And those electrodes are embedded into the socket wall. So we have limitations with sockets. So from a sensory standpoint, we have limitations from with time having his arm like his shoulder at like different angles, like hands up in the air, out to the side above his head. We can have electrodes where they would pull away from the skin, which would disrupt the signal because you have this external socket.
Rich Bennett 23:25
Right.
Jonas Seeberg 23:25
That has motion on the residual limb. So then arm gets all jittery. So we have complications and complexities with with consistent microprocessor function and then also limitation of what we would call Michelle can get into a functional envelope. So basically, what is the envelope that Tom has to work with above his head at shoulder level, his arms down at his side. So when Tom had his his arm up, there were a lot of limitations because of the fulcrum effect in the weight of the prosthesis. So it's you know, it's really hard to get above your head when you have this external socket.
Rich Bennett 24:01
Yeah.
Jonas Seeberg 24:02
And you don't have a direct skeletal connect. So by going with an issue integration and removing the socket, the two things that happened were we improved the electrodes being connected through his arms, through the external bands, which is tight, and then we've eliminated any impingement of the socket on his body that would limit motion. So we have made a lot of advancements. And then stepping down from the electrodes is just the way that we're attached now with Tom's arm is we're not dealing with an external socket that he has to contend with. We're dealing with a direct skeletal connect. So, Tom, if you tell us, I mean, you can tell us about your journey from transitioning from a socket, the limitations, and then into the surgical process. Mike For our audience.
Rich Bennett 24:49
Correct.
Tom Zdon 24:51
It's hard to kind of explain where to start, but the the first prosthetic I had was just the manual type that had a kind of a claw. It's very.
Jonas Seeberg 25:03
Body powered, not.
Tom Zdon 25:04
Powered, using your back, which was it was light. It's light, but it's kind of, you know, it's outdated for our time, right? So the second one was was the same forearm hand, but with a bucket system with electrodes as Jonas was talking. It limited me on reaching out anything to the side because it like I said, the skin was pulling away from the contacts inside the bucket. To me it was it felt like having a bowling ball strapped to the side of my arm. It was very heavy. Wow. Clunky. And then with different straps around your body just to hold it all in tight. So it's very cumbersome. You could say.
Rich Bennett 25:48
These are ones a lot of people are just putting in.
Tom Zdon 25:50
Basically what probably.
Jonas Seeberg 25:51
Most people.
Tom Zdon 25:52
Well, 95% of the people have out there.
Rich Bennett 25:54
Okay.
Jonas Seeberg 25:55
Yeah.
Tom Zdon 25:55
So so the new technology also integration is with the metal rod that's put in. It eliminates all that. And then the weight of the arm is back on your skeleton system again, where I've been wearing this now for two months, three months and it's light as a feather.
Rich Bennett 26:14
When I like having that bowling.
Tom Zdon 26:15
Ball, it's not heavy at all. Yeah, and the functions, because it has a band now that's secure on my arm, that's always making contact. It's, you know, you have much better function, right? The process right now is just still learning the the process of trying to break the nerves up.
So. So let me go back maybe three years ago, I had a surgery called Team. Ah.
Michelle Gent-Jamin 26:44
Targeted muscle renovation.
Tom Zdon 26:47
Yes. So that that's they I had a surgery. They pulled the nerves out. There's three major nerves that come from your back down your arm. You're not sure what the names are, but there's the Shriners. So they. They took them. They pulled them out. Like I always say, it's I'm a country guy. It's like an earthworm. They pulled them out of the dirt and then they split them.
Michelle Gent-Jamin 27:09
It's so helpful.
Tom Zdon 27:10
And and then they and then they put them in a radius throughout my arm. Your nerves. The nerves. So like journalists are saying, they put them close to the surface. They didn't embed them deep into the muscle, but close to the surface. So when I'm thinking about actually moving my fingers, you know, you have
I guess I don't know what you would call it, kind of like radio waves or something. Yeah. And it runs down your nerves and then it stimulates the muscle and that's what makes everything work. So I'm not like on that muscle deflection. It's actually it's a it's a brain thought pattern. You know, if I think about really moving my fingers that aren't there, my fingers move.
Rich Bennett 27:53
Yeah.
Tom Zdon 27:53
So it's with the co app system that that kind of separates it all and figures that out for you. Well and then of course with the computer day if if you get things crossed, the payoffs are crossed, you can go on a computer reverse thumb. You could have, you could pretend you're moving your arm up and it's going down. You can have it do different things with the computer tell telling the signal. So my problem right now is I'm just having to kind of relearn everything.
Rich Bennett 28:22
Right.
Tom Zdon 28:23
It's been five years, well, maybe four years or so for the arm. And it's just trying to get, like you said, 16 signals out of three nerves, trying to break up either strong signals or weak signals that will determine on different functions your arm can do.
Jonas Seeberg 28:43
So at the TMR they've separated out, basically create generating a better signal.
Rich Bennett 28:48
Okay, that.
Jonas Seeberg 28:49
The electrodes will pick up and by spacing them out you have a separation of signals. So back to the CO two, when you're listening to, to the songs that are being sung for the micro processing time is the goal right now is he has each of the patterns down, but it's separating the signals. It's hard to to describe over radio you really have to see the visual. But, but where Tom is now is he's isolating the different thoughts, He's isolating the different signals that are being received. So what we want to do is spread all of the different motor functions as far apart as we can on a map. So they're not crossing over. So if you think you're looking at like circles on a map, we're trying to keep those circles independent of one another. Just thinking if they're piled on top of each other, then you can end up with two function things happening, the two functions happening at the same time. So that's what we're working on, is spreading out that that function. And with the OCO integrated system, Tom had to go through two surgeries. So we were working with a company called Integra and the and also integration started with the Renmark family over in Sweden and we're working with dental implants and this is fascinating. Like my father's, he's retired now, but he's a dentist and back in the seventies he was doing a lot of the Renmark implants for, for, for dental purposes, for, for teeth. And it's the same, it's the same family. So the dentist son, he was a surgeon, decide to take to take osteo integration like with the abutments just on to a macro level. So they're much larger than what will go in your mouth, but it's a very similar design but on a larger scale. So Tom had to go in for surgery to have the anchor put into his bone. So it's yeah, we call it the humerus, and they had to hollow out the humerus and then put the anchor system into the bone and let it heal around the anchor once everything looked good. And and the team, the surgical team was happy with the results. Then they went ahead and created a little opening. And then they take basically a plug out and then they thread in what we call the abutment. And the abutment is what sticks out of Tom's arm. That's the metal oxide that you see. And then they and then they take the skin and they tie it back into the bone. So what Tom has is a closed system, so he has his residual limb, doesn't have any opening where the metal comes out of his body. So it is closed.
Rich Bennett 31:24
Okay.
Jonas Seeberg 31:24
So his skin doesn't weep, it doesn't drain it.
Rich Bennett 31:28
And it's okay. It just works with that. Yes. I mean, now, Don.
Jonas Seeberg 31:31
I don't think they recommend it, but we know people who do.
Rich Bennett 31:34
Okay.
Jonas Seeberg 31:35
Yeah, I have gone swimming like.
Rich Bennett 31:37
When he was.
Michelle Gent-Jamin 31:38
Swimming. Okay. Really, all they have to do is put some like aquaphor around the abutment site. They shouldn't go in any type of, like, murky water. So I don't recommend going in the Chesapeake. But if he wanted to swim in his pool, if he wanted to swim in like clean saltwater, all he would do a little aquaphor around this abutment say go swimming when he gets out of the pool, whatever clean water he's in, just wiping it down. And that that is
totally, totally okay.
Rich Bennett 32:13
I did have a question for you, but you just answered it. Yeah. So those of you listening, Tom just took his arm off. Now I can keep the.
Tom Zdon 32:20
Market off and put it on within a minute.
Rich Bennett 32:23
But what you said earlier is that that's your dominant arm. Yeah. And you're doing this with your non-dominant arm. You just took that off a new time. Yeah.
Tom Zdon 32:33
Well, you learn, you. Yeah, you adapt.
Rich Bennett 32:36
Wow.
Tom Zdon 32:37
But it's know I would say if, if amputees that are out there and they can have this done, it's it's the way to go. Yeah. It's definitely the way to go. I mean there's limitations. There's always limitations on what you can do. But, you know, four hands or something like that. I mean, this is this is really good. Mm hmm. Really good. I'm like like I said, I'm actually hoping to have my leg possibly done this way. Um, so we'll find out and find out in the future.
Jonas Seeberg 33:08
And with the surgical team, we have surgeons, like, out of Hopkins and Walter Reed that are behind working with the it's the Oprah implant system by Integra. Mm. And, and they're different team so you have your surgical team that's specific for the surgery and putting in the abutment and then you have the prosthetics team so we're responsible with working with Instagram, with the Oprah system and creating the prosthetic arm which attaches to the abutment. And then it works with Michelle that align rehab with with the functionality of the arm and what he'll be doing, like at home and in life. So to help him live the most active life possible. But this functionality is incredible. And lastly, I'll just give a plug for the Times. Times Elbow is from Steeper is the name of the company. So it's it has a robust elbow. It's very fast, very responsive. He has a motion control wrist and side. And that's what gives us the pronation and separation. And then the hand is is from a company out of Scotland that was bought by a company out of Iceland, which is, Oh, sir. And Touch Bionics is is the company acquired by Oscar. And Tom is specifically using their island quantum hands. So real life prosthetics has purchased the components from the different manufacturers around the world and have have integrated those components to design the arm that he's using today.
Rich Bennett 34:46
So with the arm. I'm sorry, Michelle, we're going to get to you here with the arm, because I'm just sitting here watching everything. It's just amazing. But how often does there does Tom need to do maintenance to it, like lubrication anything, or does it even need that.
Jonas Seeberg 35:05
Very low maintenance?
Rich Bennett 35:07
Wow.
Jonas Seeberg 35:08
Very low maintenance. I mean, for you know, for any amputee with their prosthetic limb, it's always important that they keep their limbs clean and right and debris. And so it's Tom does a very good job at, you know, taking care of his prosthetic arm. So.
Tom Zdon 35:23
Yeah, every morning I wake up, I get my shower and then I am able to get it wet, submerge it. I can it can be underwater.
Rich Bennett 35:32
Oh, well.
Tom Zdon 35:33
You know, as as it's clean, you know. Yeah. Bad bacteria, water or something, you know, it's not saying you can't go in it, but you should clean it more often. Right in the morning. I clean it with scrunchy, whatever I'm showering with. And then when I dry it off, I usually put some Vaseline or petroleum jelly or something around it. Right. And it's kind of protection for dust and dirt. And I'm active outside. So, you know, summertime is here. I'm cutting grass all the time. You know, go in the pool, wipe it down. But I think it's all about hygiene. Yeah, yeah, yeah. I guess if you're a dirty person, you're going to be dirty.
Jonas Seeberg 36:11
And Tom, speaking of the apartment, not the prosthetic arm. Yeah. So he would not want to go into the pool.
Rich Bennett 36:17
Right? Yeah.
Jonas Seeberg 36:18
Yeah, He got stuck in a rain shower. He's okay, but he doesn't want to go doing laps in a swimming pool, right? Yeah.
Tom Zdon 36:22
The arm is not waterproof. My bag is not waterproof either, But it's. It. It can be submerged. And they say it can be submerged in and just get it out of the water. Dry it off. But it's not a waterproof.
Jonas Seeberg 36:36
And we do we do build above any prosthetic legs that are submersible several meters deep that are mine. Okay. So I saw electronic function that are waterproof. But as Tom mentioned earlier, our limitations is his socket connection. Yeah. So with him, with his single handedness, the way that he puts his leg on, he has a roll on liner and then he goes into the pool. If water gets in between that liner and his skin, then it just pops off. So the systems that we use for waterproof above knee prosthetics are vacuum based systems. So so instead of you do have a liner, then you go down into the socket, but there's ceiling rings which make it waterproof and then vacuum evacuates the air. So it's suction to the amputees. Okay, so there are waterproof legs. But for Tom right now, it's a challenge. But he goes into osteo integration for his above the knee amputation. And we're getting into a whole new realm where swimming will be possible with his prosthetic leg being in a pool.
Rich Bennett 37:40
Yeah.
Michelle Gent-Jamin 37:41
I think one thing that we should mention is kind of the two stage surgery that Tom has to go through. I think you can probably tell Tom's very dedicated and very regimented in his recovery. So the the surgery is the rehab protocol is very, very specific. So after the second stage surgery, when the abutment is now installed, he had to go through a very, very, very poor, aggressive, pretty slow phase using a training prosthesis. So it was probably like a maybe a four foot
rod that would get attached to the abutment with the same system he's using here. And it came with different weights that were ranged from like 50 kilograms up to 200 grams, up to 200 grams. And he would wear those weights on the arm gradually building up to how long he was wearing those, tolerating those weights to continue to stimulate some bone growth. And then he also had to carefully load the abutment side. So he'd have to press the abutment down into a scale and try to gradually about 11 to like
£20 per day. Yeah. Pounds per day would add up how much pressure he's putting into that abutment site to again allow for the bone to really integrate into that titanium rod just as the the dental implant takes to our teeth. So he was and still is keeping track of every day I loaded on the scale up to £40. I had my training prosthesis on with 200 grams for 5 hours and I had no pain with osteo integration. They are very with the Oprah implant specific. We are very, very serious about not having pain with your training. So a pain if you've ever heard of that 0 to 10 scale, it has to be below a three. If one day he woke up and he was in a lot of pain, then either you're calling the surgeon immediately or just backing off, kind of revert to how much loading or how much weight you were wearing on the prosthesis.
Rich Bennett 40:15
Through the no pain, no gain at the window.
Michelle Gent-Jamin 40:17
Correct. That does not apply and that's not apply with. Oh, I said then once Tom was able to tolerate the 800 grams of the training prosthesis, that then made him eligible to start training with the full length prosthesis because you have to build up the tolerance to to the weight of this prosthesis. Right. So that kind of where right now in training, we are noticing a little bit of weakness in the shoulder wear, kind of maintaining the arm up over the head. You could see like, oh, man, yeah, this feels really heavy. And you could you could see have his muscles shake. But Tom has been nothing but but dedicated to keeping that protocol. And that is one thing when the surgeons and the the AU team meet, they, they really harp on, you know, this is kind of a pretty long recovery. You need to be dedicated, follow it step by step. Otherwise, there really could be adverse consequences.
Rich Bennett 41:22
So with with the therapy, especially since it's his left arm and left leg, how long is see therapy today? Because you got your knee, just the one you got to now.
Michelle Gent-Jamin 41:37
So Tom is a very strong walker. So we're not we're not doing any specific lower extremity training right now. Okay. Are just focused on on the arm. So I'd say we do it we do an hour each visit and we are working on his ability to kind of grade how much force he's putting in to pick something up and release it. So when we go to pick up, say, a solo cup that's filled with water right, we're going to approach it and put X amount of force into that cup, right? Versus if we're going to pick up a wine glass that has in it, we're going to be a lot more cautious with our grip.
Rich Bennett 42:22
I thought about all that.
Michelle Gent-Jamin 42:24
And so working on controlling that precision, he's he's kind of mastered all of the training with the elbow at 90 degrees. But then once we start to do something like reaching overhead, grab that cup out of the cupboard, right? That's where you start to see kind of some of the muscles, the signals overlapping. And sometimes he'll go forward, backward, forward or backward or I'm not doing this, and he'll say, I'm not trying to do this, I'm not trying to do this.
Tom Zdon 42:57
And it's fatigue.
Michelle Gent-Jamin 42:59
Yeah, yeah, Yes, tiring.
Tom Zdon 43:00
And then just trying to hold the arm up. It's firing off nerves that I don't want to be firing, but the arm will learn this in different programs. We can set it. It'll actually learn to hold the weight while nerves are firing off and it kind of zeros them out and then it just picks up. You could say maybe the lower signals that actually works, the fingers in the hand and everything.
Rich Bennett 43:26
All right. So, Tom, I got to ask you this. What was the young lady's name? There was.
Michelle Gent-Jamin 43:30
Joanne.
Rich Bennett 43:31
Joanne. So Joanne's thing was her, I guess, goal was she went to ride a bike, right?
Michelle Gent-Jamin 43:38
Yeah. And go up an escalator at the mall.
Rich Bennett 43:41
Oh, okay. So what actually has she riding the bike, Hit the bike?
Michelle Gent-Jamin 43:45
I don't really think that that was a serious goal, but the escalator I called her like two weeks ago and she's like, I did the escalator this weekend, so she's. She's doing it.
Rich Bennett 43:55
So what is your she? I thought she was serious about the bike. I'm sorry she was messing with me.
Michelle Gent-Jamin 44:02
I don't really I've never heard her mention the bike besides this.
Rich Bennett 44:06
You know.
Michelle Gent-Jamin 44:06
During conversations with Rich on it. So maybe she.
Rich Bennett 44:10
So she was distracted?
Michelle Gent-Jamin 44:11
Yeah.
Rich Bennett 44:12
Would you stop starstruck it? What was that noise again? You mean Michelle? The.
And it's so.
So yeah. Especially since it.
Jonas Seeberg 44:25
Sound quiet like his arm.
Rich Bennett 44:28
I think. Would you say. Yeah.
Jonas Seeberg 44:30
Flex your arm.
Rich Bennett 44:31
Time. Yeah. And now do it again. Michelle. I can't really sit here like this. Yeah, we,
I know you've, you've already done some of the things that you were doing before, like the swimmin. Yeah. You mentioned the boating too, but what are some of the things that you haven't been able to do yet that you would love to get back to doing.
Tom Zdon 44:55
Well, one of my biggest hobbies was, you know, ride motorcycles.
My opinion it's not really feasible anymore because need balance. I do have balance even just on one leg, but the way the traffic is and everything and motorcycles are just becoming more dangerous. Yeah, every day. It's not the motorcycle, it's my motorcycle fault. It's everybody.
Rich Bennett 45:20
The four wheelers around you.
Tom Zdon 45:21
Yeah, but I have rode pedal bike. I can ride a pedal bike.
Rich Bennett 45:27
Wow. Okay.
Tom Zdon 45:28
You know, with with my prosthetic leg, even without my arm. But it's stopping and starting, you know, where my falling. That's the problem. Because if the bike starts to lean to the left, I don't have a left leg. I'm just going to fall right over. But I can ride a bike and maybe I'll just have extra good balance. Like I said, I was a water skier, right? All the time. I went out last year, I water skied on one leg. Wow. So if there's a will, you can do it if you want to do it. So I'm not really sure what I want to do actually now and what my goals are. The big thing is just trying to get back to you could say normal again. Yeah. With the with this arm, it has definitely helped me in the last three months. Just as doing simple things is making preparing dinner, holding a dish down,
holding a thing of lettuce down while I'm using my other hand to cut it up. Walking out to the mailbox. One big thing with me is I have to have a cane because my leg is cut up so high. I don't have balance on it no more. So my good arm is always pretty much used as my cane. Now I can walk without a cane, but I'm kind of like hopping.
Rich Bennett 46:51
So you want to avoid.
Tom Zdon 46:52
So with this hand in the way it is, you know, sometimes it's kind of cumbersome, but with the Oh, I now it's it's kind of becoming part of your life again, right? It's starting to feel a little bit more normal. I carry my mail, I carry groceries, I can put bags in it, I can carry. And then again, it's it's I'm still learning the process of training it through my brain and through the signals, you know, carrying something heavy. I don't want to drop it. So I'm constantly trying to think about it. Hold my arm up, hold my arm up. But I would say it's probably 5050 because there's a lot of things I do now that I don't even think about it, and it's already doing it for me.
Rich Bennett 47:32
Yeah.
Tom Zdon 47:33
So it's kind of like becoming your seventh sense again.
Jonas Seeberg 47:36
And my aunt, I was going to ask that. So in the beginning, like really working on bending my elbow, bending my elbow, this is the specific signal that I'm sending. So you're saying now you're not really thinking.
Tom Zdon 47:47
About if I just want to stop, I just.
Rich Bennett 47:49
Ended up right.
Jonas Seeberg 47:50
So like playing a piano, right? So you have to learn the notes, but then you start playing songs or keyboarding on a computer. Yeah. You know, these are the different keys and you just think in words. And I will elaborate more in the hand. So this island quantum hand is, is a very, very complex hand. So you can see individual finger motions. So for fingers and thumb, so the fingers will open and close and the thumb will actually rotate around like four different grip patterns. And with this hand there's 24 patterns, up to 36 that we can assign. So you think of our hands, you look at your hand. There's a lot of you can take your hand through to grab different objects. You know, as Michelle was saying, if Tom's grabbing a wineglass, you know, there's a specific pattern to that. So he has to have it, you know, hand open, come up to it and close the hand down. There are there are storm motors in each individual finger. So so say the stem of the wineglass as soon as pinky ring finger, middle finger index finger come into contact with the stem, they will stall. So he won't continue to squeeze the glass and then the thumb and the index will continue to wrap around the glass. So this hand, it doesn't take a lot of power to hold an object. It just has more control over the object, by the way, that the fingers hold and take the shape of the object that Tom is holding. So the different grip patterns allow Tom to, you know, move into if he's, you know, going to keyboard with his index finger, if he's going to hold a credit card, we call it like a lateral grip. This system is unique. One of the reasons we used it is it has it's a it's called like a gesture control. So Tom can Tom can set his prosthesis in a certain position and then shift his arm forward quickly, backwards, quickly inward, quickly or outward, quickly. And each of those motions will automatically move the hand into a different gesture that he wants to use. And then beyond gesture control, we have what are called grip chips so we can set a grip chip next to a keyboard. So Tom comes in a proximity of that grip chip. The hand will move into a position where he can keyboard. If he's in as if he's in his kitchen, we'll set a grip chip in the kitchen. So he would move into gesture. That would be good for a holding utensils. So. So it will automatically like quickly move into that grip pattern so he doesn't have to think about it close. So that's that's one of the big reasons in choosing this hand is with that gesture control and that grip chips.
So so that's just to.
Michelle Gent-Jamin 50:27
Manually.
Jonas Seeberg 50:27
Enrich you can with with width estimator. Just to give you an idea of how precise estimators are, Tom could pick up a blueberry and not crush it. So you got to pick up the blueberry. You while you would have you would have the thumb and the index finger coming together and then stop on that blueberry between squeezing it. Then, of course, if he wants to crush it, he squeezes it and he can crush it. If he's shaking your hands, he can shake your hand. His hand will wrap around yours and not crush your hand unless if he wants to.
Rich Bennett 50:56
So he can crack a damn walnut with them. Yeah, yeah, yeah. Wow.
Tom Zdon 51:01
I'm still learning it. Sometimes the signals are still going a little haywire, Right? But, yeah, you know, with time, it's going to. It's just going to click and it's all going to be there.
Jonas Seeberg 51:11
And if he's carrying something now, we have a direct skeletal attachment, which is incredible. So if he's carrying something with his hands, say like a like a briefcase.
Rich Bennett 51:20
Yeah.
Jonas Seeberg 51:21
Like he can he can control that briefcase handles with the hand with four fingers wrapped around it and then the thumb making the block on the other side. And we have a direct skeletal attachment so we don't have a socket that's pulling away from his body. And each finger takes takes close to £15 of pressure. So. So he has close to £50 that he can carry without his fingers detaching from from the Palmer section of the hands.
Rich Bennett 51:47
Wow.
Jonas Seeberg 51:49
And if he does break a finger, we could remove each finger individually to fix it. And to replace it.
Rich Bennett 51:53
Don't have to put it in splint. No, no.
Jonas Seeberg 51:56
No. We just replace.
Rich Bennett 51:57
That is amazing.
Michelle Gent-Jamin 51:59
Yeah. One really cool feature with with the arm in general and just upper upper extremity prostheses in general is he can go into kind of like a free swinging mode. So when you and I are walking, right, we have this natural.
Rich Bennett 52:14
Begging.
Michelle Gent-Jamin 52:14
For arm swing. So for someone who's not using a prosthesis, their arm swaying, it's it's, it's lacking. Right. And also can throw off can throw off balance a lot now that Tom kind of has this the symmetry with this arm swing I would expect that his balance when he is wearing the prosthesis will get better as as he's walking as as our bodies were designed to do.
Jonas Seeberg 52:42
So as an above the knee amputee just the arm swinging upper extremity you're saying will generate more power for his above the knee.
Michelle Gent-Jamin 52:51
Yeah that's the best the rotational.
Tom Zdon 52:55
Work think it does, but it just just that little bit of weight makes me walk a little bit more.
Rich Bennett 53:01
Straighter.
Tom Zdon 53:02
Not kind of lean in or something. You know, we're all kind of designed equally split right down the middle, both sides. So it does help you in balance.
Jonas Seeberg 53:11
Wow. I think we have a twist. So you think when you're when Tom's right leg is forward, his left arm is forward and vice versa. So now he has when his left leg is coming forward, his prosthetic leg, he has that trunk rotation and the arm swing and the way to the prosthesis like to bring his mechanics.
Rich Bennett 53:28
Together, see little things like that. People don't think of people more or less take it for granted. You know, and then you're now you got to learn basically how to do all that over again, right?
Tom Zdon 53:41
Yeah. I mean, definitely with this. Oh, I is it's the way to go. Yeah. Especially on a one an arm or a leg. I mean, there's many people that have been going through, you know, 20 years with different type legs and, you know, it depends on the situation. Plus with the the eye I a leg which I'm hoping maybe to have we don't know yet. Doctors have to see if I have enough bone.
Jonas Seeberg 54:10
You were just in yesterday. You said you're just.
Tom Zdon 54:12
Down at Johns Hopkins yesterday and a bunch of x rays. And you know, there's limitations on that, too. You know, I'm a I'm an active person.
Rich Bennett 54:21
Mm.
Tom Zdon 54:22
With oh, oh, I in the leg. Am I still going to be able to do a lot of the things that I could do because it is kind of like I kind of picture this metal rod in the bone and it's like taken like a number two pencil. You're putting that stress on that bone where you can see a pencil kind of bend a little bit. You know, normally you have your your muscle and your skin all around it. So you have you know, it makes it a lot stronger. But your bone is very strong. You know, it's stronger than you think. It's not like you could just take it out and crack it in half. Yeah, but but, you know, with having a rod, especially like with the arm, when I'm carrying weight on it, all that weight is right on that rod in that bone. It's not really, like connected through all your ligaments, your forearm, everything. So there is a limitation on that. So with the leg, I got to really figure out some options. You know, is it going to benefit me? Is it not? You know, is the bucket going to be better? Yeah. And it being my lifestyle, I do a lot of things that probably prosthetic people shouldn't be doing. I still go up and down ladders. You know, I shouldn't be doing that at all.
Rich Bennett 55:35
But
that's.
Tom Zdon 55:38
The way it.
Rich Bennett 55:38
Is. And Michelle's like, It's not true. You can't. It's okay. You can.
Tom Zdon 55:44
You know. But. But yeah, it's it depends on what you want to do. Yeah. What you want to do. You know, I can, I can say, you know, if you're, if you're in your sixties or seventies and you went through diabetes and, and which I guess most cases are probably with most amputees or probably diabetes of losing limbs.
Michelle Gent-Jamin 56:04
54% vascular.
Rich Bennett 56:06
Is that what it is? 54.
Tom Zdon 56:09
Yeah. And I think a lot of it is being in shape, especially if you're if you're in shape and you're not overweight. It all plays a factor that definitely.
Rich Bennett 56:19
So something you mentioned earlier before we started recording. And I want you to explain this to everybody, because this, I'm sorry, pissed me off with the driving. Yes. Because you basically had to what? You had to you couldn't you couldn't drive that you were saying you had to go through?
Tom Zdon 56:39
Yes, I had to go through a bunch of relearning ability. Of course, this is the state of Maryland. So every state is different. Right. But the state of Maryland is if you lose a limb
or a leg, you're required to go back through a driving school that you have to pay to learn how to drive again, learn like you're testing just like you were like you were 16 years old again, to go through all of that, it's a process. And then you think you would have the okay to get your license back and then you have to go to the NBA and do all that over again. So it's like a two part thing. Now, other states are different. You don't it doesn't matter what like you, you lose. You can still drive. Of course, if it's a clutch car, you know, then then you got big problem. But most cars, more clutch is no more.
Rich Bennett 57:33
Yeah. Those are called, we call them anti-theft devices. Now you.
Tom Zdon 57:39
But you know, I mean like you said it's a it's a willpower. Yeah. You know if you want to do that you got it. You got to go through two classes. You got to do it,
and it gives you your freedom back because it's it's nice to just be able to get in your car, drive somewhere else, go adventure out, You know.
Rich Bennett 58:00
The thing it gets me is the and I guess what really irks me about that, though, is if some guy's got a full leg cast on, they don't have to go through it. They could still drive. And I only knew that because I was watching that, you know, which was kind of hard to do with one leg. Yeah.
Michelle Gent-Jamin 58:20
Yeah. And so my, my, my biggest beef with it is, is really the insurer doesn't care what you're doing outside of your home as long as you are independent inside of your house. Then in their eyes you are you were good. So for them to to pay for driving school, well that means that you're actively leaving your house. So we're not going to pay for that. So all of this is is an out of pocket expense. My gosh, in the state of Maryland, I think there's maybe five, five driving schools. Two of them are hospital based, three are independent. You have to have a formal evaluation by an occupational therapist to first kind of check you off and say, yes, you you have the qualifications to drive. Then you have to go through the testing, say someone needed adaptive pedals. They they needed hand cranks. You go, you try out all the different equipment, each training session you do with the different equipment. It's running about 125, 150, $50 per visit.
Rich Bennett 59:20
Per visit, per visit.
Michelle Gent-Jamin 59:22
Then you have to go and you have to purchase the adaptive equipment if were you to need it and then go back to the DMV and take your your formal driving test, there's a whole host of different doctor's visits that people have to go to get checked off. Some of my patients, most recently, they were talking about they they put you through cognitive exams. So, you know, you lost a leg, right.
Cognitively, you wouldn't think anything would be majorly impaired. Right. We're not we're not doing random cog screenings on, you know, older adults who are driving. But just because. Yeah, now you're missing a limb, you have to go through all of this extra training just for you to move on with your life, for you to be able to drive yourself to the grocery store or get your groceries and go home by yourself. They're really it's just a huge barrier. No, you need to call someone to come pick you up so that they can take you to the grocery store and where you weigh on them. So it's it's yeah, it's really just another obstacle impeding patients, getting their independence back faster.
Rich Bennett 1:00:33
Okay. So then when that happened with you, Tom, because last time we talked Transportation's a problem. How were you getting back and forth?
Tom Zdon 1:00:44
I after my accident, fortunately, I never really went far once I finally grew up. So my mom is still alive and I stayed with her. Okay. She's about two miles from my house. So for about 6 to 9 months, I pretty much stayed where I grew up at my mom's house, so she was pretty much my caretaker.
Rich Bennett 1:01:08
Okay.
Tom Zdon 1:01:09
If you don't have that option, then, you know, that can put you in a home somewheres or having a provider to come out in your pocket expense. Yeah, Yeah, yeah. I don't know. It's I know every the world revolves around money. Yeah. Everything is money issues. But, you know, if you got the will, you're going to figure it out. So the first chance I had to finally get back out of my mom's house, I went back home. I've been in my house for 25 years, so, yeah, you know, once you're out on your own, you're out. But it's it's it's nice to have family members help you or, you know, any help you can get. But it is a big change of life. It's a big change of life.
Rich Bennett 1:01:53
And and like you said, too, not everybody has.
Tom Zdon 1:01:55
And not a lot of people can deal with that and they need help. It needs to be more help out there for people.
Jonas Seeberg 1:02:03
I can say is Tom's processed like just being on this journey with him from the beginning. It was incredible. Just his family support, his mom, his sisters very much, you know, encouraging him, surrounding him. So just seeing his journey of and again, he's so fortunate, you know, just to have this, you know, to see his family really care for him. Well, to motivate him to to to then see them disappear. It's like in the beginning they were at the appointments and then they disappeared. And then Tom was back at home and he had regained his independence. And it's just amazing seeing Tom's transformation. And so.
Tom Zdon 1:02:43
Now it's a lot I don't I don't think a lot of people could go.
Rich Bennett 1:02:46
Through it. Yeah.
Tom Zdon 1:02:47
And I wouldn't want nobody to go through what I've gone through so far. But I mean, it happens. It happens every day. Every minute. There's somebody out there, somebody getting in a car accident and, you know, losing limbs. And it's it's gotten better.
Rich Bennett 1:03:03
You're driving now, right? Yes.
Tom Zdon 1:03:05
Yeah, I've been driving for the last about I would say close to maybe nine months. I was out of commission. Okay. Until I finally got my first leg through real life prosthetics. That's when I started driving again. I do not drive unless I have a leg one. Okay. You can. You can use a wheelchair, roll over to it, get in the car and go. But that's just not me. Yeah, it's not. If I'm not going to drive, if I don't have my leg going. So because you don't know the situation
just the way I am.
Rich Bennett 1:03:38
Something you mentioned earlier too, is the support groups you said you were going to offer. Is there any other support groups?
Tom Zdon 1:03:46
There are at different locations. I went to KERNAN, which is around the Beltway, but I mean, being here in Hartford County and Aberdeen is where I live. That's that's a long journey to go there for just a one hour session. I haven't yet to do that in the last four years, but I would like to go down it at least it's a it's a good way to meet people.
Rich Bennett 1:04:09
Yeah.
Tom Zdon 1:04:10
To try to talk to different people. And there again, I'm a person where I don't really need support. I'm going to do it on my own. So everybody's got their own individual. You know, they're they can cope with way they're doing it.
Rich Bennett 1:04:26
Yeah.
Tom Zdon 1:04:28
Maybe I could be left alone. I'll survive. I'll be good.
Rich Bennett 1:04:31
Here's here's what I was thinking, though. I think with you and your story, I think there's a lot you have to offer to other people. Yes. Have you ever thought about it? Don't lay for me about this. I'm serious. Have you ever thought about going and speaking to groups?
Tom Zdon 1:04:52
I mean, I would. I would. It's a learning, you know, nobody likes to get in front of a lot of people and talk. Yeah, but it it doesn't bother me. And if I feel like I can help somebody out there, it does make me feel good, you know, because it's a whole new chapter in life. You know, it might not been like this years ago. Pretty much. You know, just leave me alone. Let me do my own thing. But. But now, if I can do something to help because I am considered 100% disabled, I could go out and get a job. But for right now, I am collecting Social Security, disability, and any kind of income that I would get would kind of mess everything up, right? It's it's very hard to get social Security disability at a younger age. Um, but I'm luckily I'm getting something back through all the years that I've worked. Yeah, but yeah, like I do go like I said, up to Upper Chesapeake. I talked to a couple of different people. I mean, I help what I can, but are I don't need somebody complaining to me because I'm not going to be there for them.
Rich Bennett 1:05:58
Yeah.
Tom Zdon 1:05:59
You know, I'll help them that much. I can. I'll go out of my way a couple of times. But if I don't get feedback, you're on your own. And that's, that's just me talking.
Rich Bennett 1:06:08
Yeah.
Tom Zdon 1:06:09
So, but I've, I've connected with a couple younger people maybe my age has had a couple amputees or something, and I kind of reached out to them a couple of times and but they just had anger issues and, you know, it's not for me. Yeah. So, you know, I try to help them out. And if they're going to be angered that I'm not going to be around it.
Rich Bennett 1:06:32
My thing is what I think you would be very good at is, yeah, it does take time to learn how to talk in front of people. Yeah. I mean, took me a long time.
Tom Zdon 1:06:43
And we're still learning each.
Rich Bennett 1:06:44
Day. Yeah, the train, it never stops. But what I'm thinking of, because when it gets warm out, you get everybody out on their bikes and you start seeing the accidents, which is something I hate seeing. Yeah, but if you could get out and talk, I would say even at the high school level, because that's get them when they're young. Yeah. You know, And now you got to be, you got to be mindful of everything. That's right. I quit. I quit riding when I myself hugging my tank. And if I'm hugging my tank, then it's it's time to get rid of the bike. I'm not riding anymore because it's what's around you. You never know. Yeah. You know, and especially when people are driving the day. I mean, people could be spilling their coffee and just you, you never you just little people are still on their cell phones. Well, nobody.
Tom Zdon 1:07:38
Knows the.
Rich Bennett 1:07:39
Time. Yeah.
Tom Zdon 1:07:40
What Hands off. You know, we're not supposed to be touching anything. But now the cars had these big computer screens on them.
Rich Bennett 1:07:46
Some of them even have freaking Netflix on it.
Michelle Gent-Jamin 1:07:48
I have seen that. I have seen.
Rich Bennett 1:07:51
You talk about distracted driving, but you got Netflix. Oh, we can't watch you while you're while you're driving the what the hell in order for first of all. Oh yeah it's like you.
Jonas Seeberg 1:08:01
Slow in the passing lane.
Rich Bennett 1:08:03
And it's like this.
Jonas Seeberg 1:08:05
Lane is for passing and you go in the speed of everybody else because you're not looking at the road.
Rich Bennett 1:08:10
And it peripheral.
Jonas Seeberg 1:08:12
Vision driving.
Rich Bennett 1:08:13
It baffles me. It's like, yeah, we got to get away from distracted driving. Then we're using the cell phones. Oh, Facebook on my screen. Okay, good message.
Michelle Gent-Jamin 1:08:23
But I.
Jonas Seeberg 1:08:25
A nonprofit organization, Amputee Coalition of.
Rich Bennett 1:08:28
America. Oh, really?
Jonas Seeberg 1:08:29
Yes. And they they do have amputees where you can go through a program, get trained, and you can get certified to to travel to different hospitals, to speak to amputees that are going through amputation for the first time. So, you know, as humans, I mean, we're we're we're needy and we're needed, you know, and thinking of, you know, a veteran like Tom who as who has been through the doldrums, who has come out and who is living life with ability, again, going and meeting somebody who's gone through an amputation surgery for the first time, who's scared. There's lots of unknowns. Yeah, how powerful that is for Tom to be there, to speak one on one and to motivate and let them know there's life beyond amputation. It's huge. And I feel that that's something that we are lacking in Harford County.
Rich Bennett 1:09:15
I would say everywhere. Yeah.
Michelle Gent-Jamin 1:09:18
Yeah. And Tom speaks so eloquently, I, I, my personal goal for Tom is to, to be like a patient ambassador or rep for the you integration implant. So when Tiger on that these big conferences where a lot of amputees are walking by Tom is standing up at their booths showing like this is what I have, this is how successful I've and just.
Tom Zdon 1:09:42
Help you know. Yeah, yeah. You know, like I said, everybody's different.
Rich Bennett 1:09:46
Yeah.
Tom Zdon 1:09:47
You know, if I can help somebody and it makes me feel good, I mean, I think that's the goal I think of is so it's, you know, it's a challenge. It's a challenge every day. And, you know, the other thing is, is you know, it's almost five years for me now, and I feel like I'm finally starting to calm down to where I'm kind of enjoying my life again. And it works different with everybody. I mean, I still have terrible phantom pain, which is, you know, I'm still feeling the limb loss. My feet, my yeah, I feel that every day. Now, some people say it goes away sometimes it will always stay with you. I, I personally think it's probably always going to stay with you being it was my left hand, my dominant hand. I mean, I feel my fingers every day. And I. I feel like I'll probably always feel that. But I don't have the shooting pains and the the other symptoms that are going on. So you do have to tell yourself it's getting better. And it is. Yeah, it is. I might not say it sometimes, but, um, over a period of time other people see it, so you got to believe in it. You got to. Yeah. You got to keep pushing on.
Jonas Seeberg 1:11:02
I have a question time, you know, So now that you've been wearing this arm, if you have phantom pain in your fingers and you're wearing your arm, where do you perceive that pain? I am the prosthetic hand.
Tom Zdon 1:11:15
I do feel it a little bit more. It does feel like I'm above above elbow amputee. So it used to feel like my fingers were like right there within five inches of actual amputee amputation. But when I wear this arm and with the cuff around it, it's kind of putting pressure. It does make you feel like my hand is growing. It makes it feel like the sensation of my fingers that I feel they feel like they're actually starting to grow, right. They're starting to go back to where they used to be.
Jonas Seeberg 1:11:50
What level are they now, if you around what level?
Tom Zdon 1:11:54
I would say I would say I was always at kind of like a three from a one to a ten and everybody takes pain different.
Rich Bennett 1:12:03
No, no, no.
Jonas Seeberg 1:12:03
No, not, not pain. But but if you're you felt like your fingers were closed.
Tom Zdon 1:12:08
Well, they used to felt like. Yeah, they used to feel like they were like in my elbow all the time. But now they feel like they're maybe halfway, like almost my.
Rich Bennett 1:12:15
Okay.
Tom Zdon 1:12:16
Getting closer to the wrist and it works different. Maybe that's the way the sergeant, when he cuts your nerves after an amputation, how they redo it. If it's if your nerve, they say your nerves always grow. If your nerves grow up to a eighth inch a year, they could grow because they're trying to find their home again now. And sometimes patients will have what is called as a neuroma. Your nerves will grow and they'll grow into a bunch like ball and then you'll have to have surgery to cut them back out. So until your nerves and your body feels like you're you're a calm and your fingers are kind of back to everything. Mm hmm. Your nerves will actually stop growing, they say. So as far as my leg, I always feel my. My feet burn and my toes are burned and tingling. But for me, they've always felt like they're in the same spot right? I don't feel it at my stump, at my leg. I always feel it at my shoe. I feel like they're inside my shoes or in my prosthetic foot. They're in that foot. They're down, they're burning.
Jonas Seeberg 1:13:31
So. Well, the same thing happened with your hand. I'm wondering that.
Tom Zdon 1:13:33
So kind of there's no translation.
Jonas Seeberg 1:13:35
All the way down to your fingers.
Tom Zdon 1:13:36
So it does feel like it feels like and I think it's more a brain thing going on. Yeah. You know, you see your hand moving all the time, so your brain's going to tell you it's there. It's kind of like going through a mirror, mirror therapy to where you're kind of mimicking your other half of your body. Mm hmm. I've tried that, but I guess you have to be a believer. You know, I'm not. I just. I don't believe in a lot of things. I got to. I'm just one that's got to see it to believe it.
Rich Bennett 1:14:05
Well, how are you laughing?
Michelle Gent-Jamin 1:14:07
Because it's. It is so true. And when we are teaching a patient how to do mirror box therapy, you're pretty much you're you're placing a mirror. If it's above if it's a lower extremity or upper extremity, you're placing the mirror to face the intact limb. And the intact limb is going to make different movements and the is watching in the mirror to see their reflection. So it's it's mimicking as if it's mirroring the like now missing extremity.
And, you know, there's no there's no true cure for this phantom pain, phantom sensation. It's just one arm technique that has shown some success. But it's a very specific there's no true like dosage of mirror therapy. So you should it, you know, 15 minutes at a time, four times a day for two weeks to get the optimal result. You know, how much buy in is someone going to have like I'm going to look a mirror moving my hand for 15 minutes, four times a day for two weeks. The buy in typically is not there. So it's on the provider. You know, how can we how can we word this to maybe, you know, really persuade someone to to to try it. But yeah, there's there's really not a one size fits all as far as the the phantom management but.
Tom Zdon 1:15:34
I would say try anything try, try anything. And if it works for you, that's it's great.
Rich Bennett 1:15:40
You know.
Michelle Gent-Jamin 1:15:40
Got to.
Tom Zdon 1:15:40
Believe somewhat the same We all should be the same. We all breathe and you know but but we all do have different brains, you know, And this training is training your brain to to kind of calm things down again. Yeah. So but, um, yeah, it's, it's, it's there.
Jonas Seeberg 1:15:58
And then back with the prosthetic build. We talked about the past with the old sockets and then the present with what Tom is currently wearing. And I believe the future, what I've been told is we're going to get even closer to Luke Skywalker and that the Coapt ban that's wrapped around Tom's residual limb. Right. You can see the 16 cables going down into the microprocessor unit. The surgeons are going to look into tying wires from muscle from nerve to pick up a signal internally and then bring those wires down through the abutment. So if you're looking at the bottom of the abutment, you can see the connection points. Yeah. So then when Tom connects his arm, it's a direct connect from body prosthesis and you're eliminating the external cuff and wiring.
Rich Bennett 1:16:54
Oh wow.
Jonas Seeberg 1:16:55
So that will be to see in the future because.
Rich Bennett 1:16:59
This is great because very near future.
Jonas Seeberg 1:17:01
Because then Tom won't have the constriction of the cuff, like grabbing on his muscles, pinching his arm, possibly triggering some of this like phantom, you know, the phantom sensations. And I mean, that.
Tom Zdon 1:17:12
Issue that they actually talked about that I think it was called the E implant. But the problem was, is they're still developing as it only had so many connections. I think it maybe had six, six pins on it. Okay. Where here I have 16.
Rich Bennett 1:17:29
16 year.
Tom Zdon 1:17:30
16 connections. So I'm getting 16 different signals compared to only maybe six. But as technology goes on, it's going to keep breaking up with more computer software and everything and, you know, anything. Eliminate a bucket that's around you, you know, a cough, anything that restricts your body and has you back to somewhat normal.
Rich Bennett 1:17:55
Yeah.
Jonas Seeberg 1:17:55
And there is another line or base system that we just started using, and it's a it's a line that rolls up on to the skin and the electrodes are inside of the liner and that's down to six or eight electrodes. So it's half of what Tom has and it's still the coapt technology. So it may be that when they go to that next phase of the implant that they're maybe six seven wire leads for the connection.
Rich Bennett 1:18:20
Wow.
Jonas Seeberg 1:18:21
It's exciting.
Rich Bennett 1:18:22
It is. It's amazing. It just it's I keep thinking to, you know, as a younger kid, looking at the popular science magazines, you know, the get the the show come out $6 Million Man is like, yeah, yeah. So this is never going to happen. And now here it is. It's happening. Mm hmm. Yeah, it's right before our eyes. Yeah.
Jonas Seeberg 1:18:44
In this age.
Rich Bennett 1:18:45
It's just a.
Jonas Seeberg 1:18:46
Mythology is advancing so fast. It's amazing in the last five years and prosthetics and how much has come to the market and all the options we have to integrate into prosthetics systems. That's absolutely amazing.
Rich Bennett 1:19:00
Tell everybody the websites, because that's important. Well, Tom doesn't have a website. I mean, for real life, we're five miles long so it's.
Jonas Seeberg 1:19:10
WW w dot real life prosthetics dot com.
Rich Bennett 1:19:15
That's not that long.
Jonas Seeberg 1:19:16
Our real life
epr0sthet ics dot com.
Rich Bennett 1:19:23
I want you to weigh in on.
Michelle Gent-Jamin 1:19:28
And then for align rehab we are a line rehab dash PTO icon.
Rich Bennett 1:19:35
See, that's more because it's got the dash the dash.
Michelle Gent-Jamin 1:19:38
So is it a slash? Is it a dash.
Rich Bennett 1:19:41
Or do you spell out.
Michelle Gent-Jamin 1:19:42
Dash? Exactly. So it's just the range between the letters dash. Good as I can describe.
Jonas Seeberg 1:19:50
Not spelled out. It's the dash.
Michelle Gent-Jamin 1:19:52
Or if you go to Google and type in a line rehabilitation amputee specialists, it'll pop up to.
Jonas Seeberg 1:20:00
And that's up.
Rich Bennett 1:20:01
Here. Just look for the links in the shirt. Yes. GZ is way.
Michelle Gent-Jamin 1:20:04
Multiple methods.
Jonas Seeberg 1:20:06
And that's a boom on urn.
Rich Bennett 1:20:07
Does anybody have anything to add?
Michelle Gent-Jamin 1:20:10
Oh, one thing I did want to comment on as far as the the support groups is one of my, my big dreams now with with my new facility is to be able to facilitate a supportive environment. Don't want to call it a support group, but either, you know, a bi monthly group, fitness class or just a bi monthly like, hey, anyone? I like all of my patients come hang out here. Kind of more of a social hour, right? So we're we're not just sitting around kind of talking about the and I want to put words from other people's mouths, but like the woe is me, you know, I can't do this. I can't do that. This is what happened to me. For some people, that's not therapeutic right. It's it's kind of depressing to hear that. But to just meet other amputees that are in Hartford County and socialize and make friendships that way. That is something that I really look forward to doing. Even like right now in my office in Delaware, I've had one patient who he was just really struggling. He came in on a Tuesday, so that was a I'm done. I don't see a future of myself using this prosthesis. I just can't figure it out. So I call my patient and I'm like a different patient. I'm like, Hey, John, do you mind, like, reaching out to my patient? You know, he's really down in the dumps and just he this gentleman is just so motivational. So he did. He called them, like, text back. He's like, Yep, I'll be there. His Friday session, too. So he comes in to Friday. He's just hanging out. We're just we're working on getting on and off the floor. My patient really needed to clean out of his tractor, the gumballs. All he was. He was saying, I can't. I have to clean my tractor. So many gumballs in it and I can't do it. So that Friday, when both patients were together, I was like, All right, we're getting on the floor. Get on your back. And start pretending that we're working overhead. And that's what we did. So Monday I get videos from his wife over the weekend, and sure enough, he is out in the garage transferring to the floor. The tractor's lifted and he is cleaning the gumballs out. So we went from Tuesday to life was over to then meeting an amputee who's been there, done it been successful, can show him there is life after amputation to now over the weekend doing the thing he said there's no way I can ever do this again. Wow So the power of peer support is it. It can. We need to have more of it. And it is just such a wonderful environment. And I now have patients. I'm like, Oh yeah, I come in early. So like you, you can chat. Like when, before you guys are leaving and they're talking about their different sockets, the things they've tried out, like, oh, you know, someone told me this. Yeah, they'll never understand what it's like. And just hearing them dialogue, it's such an uplifting environment that I think being able to now start doing that more regularly in a non like, Oh, it's on schedule, more of a outlook, come hang out and socialize. It's something I'm like very, very because.
Rich Bennett 1:23:23
That's a great idea. I mean in, in the new area you could put like a little coffee room.
Michelle Gent-Jamin 1:23:29
I know I was like, I think I'm going to get couch like, I want to get a couch. I don't know. Thanks for your chairs.
Rich Bennett 1:23:36
Yeah, we'll talk about that. We'll talk about that a little bit.
Jonas Seeberg 1:23:39
It's in. I would say it's like if you're an amputee out there and you do have a prosthetic limb and you do feel like there are limitations from a step fit standpoint, function standpoint, you don't feel like you're living your life as actively as you should be.
Rich Bennett 1:23:55
Mm hmm.
Jonas Seeberg 1:23:56
I mean it. Give us a call. You know, go to that website, press the button. It takes one click of a button. And if anything, come in and let us take a second look, you know, on our teams. I mean, we have prosthetist, physical therapists working side by side and just a look at your whole picture, you know, what are you doing? What are your goals, what are your ambitions? And we can evaluate to see if there are other options for you. And but that's what we're here for. So we're definitely here for our resource, you know, as a resource and to and to help you live your life to your to your fullest journeys.
Rich Bennett 1:24:31
Michelle, I want to thank you both. Tom, thank you for sharing your story. And, you know, I think you have a calling to go out and talk to people. I just incredible. Yeah. Yeah. It is easy hearing from.
Tom Zdon 1:24:46
Yeah, if I can help somebody, you know, we're glad we're glad to help somebody.
Jonas Seeberg 1:24:52
The reality is we try to keep up with Tom. Yeah, He's so far out there. Like, technology wise, it's like he's going for the latest and the greatest.
Tom Zdon 1:24:59
And it's like.
Jonas Seeberg 1:25:00
The professionals are, Okay, we're going to learn from.
Tom Zdon 1:25:02
This guy. Any hobbies? I don't ride a bike, but I still have my boats and a bunch of hotrod cars and all. And, you know, I got the swimming pool, so I can do cannonballs and carry pellets.
Michelle Gent-Jamin 1:25:14
He has pellets on his shoulder.
Tom Zdon 1:25:15
I carry I carry £40 bags, pellets from my truck in to to house up steps. You know, if there's a way, you'll figure it out. You'll find it, you know, if you want to if you really want to do it, you know, there's a way to do it.

Rich Bennett
Host
Alicia Hamilton
Co-host
Colleen Curran
Co-host
Dani Pettrey
Co-host
Derek Pentz
Co-host
Jennifer Hathaway
Co-host
Joe Ayler
Co-host
Julia Chang
Co-host
Paige Mullhausen
Co-host
Wendy Beck
Co-hostPodcasts we love
Check out these other fine podcasts recommended by us, not an algorithm.

Mouthful of Graffiti
Mouthful of Graffiti Podcast
Harford Business Beat
podcast
TRUTH Be Told Podcast
Trinity Productions - A Multimedia Ministry of the Voice of Truth Center
Spirit Speakeasy
Joy Giovanni
Podcasting Made Simple
Alex Sanfilippo, PodMatch.com
Buzzcast
Buzzsprout
TMA Connection
Tim Markland
I Have A Podcast by Vinnie Potestivo
Vinnie Potestivo
Mentally A Badass
Justine Rodes
From Survivor to Thriver
Erik DaRosa & Marc Fernandes
Chatter Box Radio
Carrie Farris
Healing #Nofilter
Laura Renner
Tools of the Podcast Trade w/J. Rosemarie Francis
J. Rosemarie Francis
The Proffitt Podcast
Krystal Proffitt
Creating Joyful Readers
Samantha in Secondary
#RockStarLife: Coffee Break
Zenobia Darling Creative